Contents

Where will my labour be induced?
You will be invited to come to the induction suite in Aberdeen Maternity Hospital to have the process of induction started. If you live close to Dr Gray’s Maternity Unit, Elgin you may be invited to attend there first for the cook balloon to be inserted prior to attending Aberdeen.
When will an outpatient induction be an option?
Women with low risk pregnancies who have a cook balloon inserted as the method of induction will be able to go home during the initial stages of the induction process, this is known as outpatient induction.
An outpatient induction of labour:
- Reduces the amount of time you will need to stay in hospital before your labour begins.
- Allows you to stay at home which evidence has shown helps labour to progress as you are in a familiar place.
- Makes the process of induction as close as possible to going into labour naturally.
You will have to stay in hospital if your induction is for a medical reason or if the method of induction used is a Prostaglandin pessary. This is to allow staff to monitor you and your baby at periods throughout the induction process.
What happens when I come in for induction?
On arrival a midwife will do a full antenatal check, perform a tracing of your baby’s heartbeat and discuss the induction process. A vaginal examination will be carried out to assess if your cervix is ‘favourable’ to have your waters broken (Artificial Rupture of Membranes). If your cervix is not favourable then one or both of the following methods may be used.
What methods are used if my cervix is not favourable?
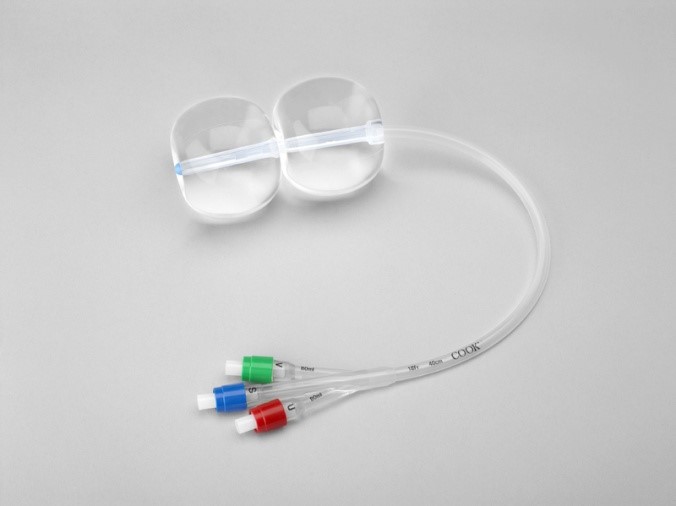
Cervical Ripening Balloon Catheter
This is the only method used for outpatient induction of labour. This is because it has minimal side effects and does not need you or your baby to be monitored as closely as when using a medical method. The procedure involves inserting a catheter into your cervix. It consists of two balloons one of which rests on the baby’s head and the other sits in the vagina. Both balloons are filled with sterile saline (salt water). The catheter remains in place for a minimum of 12 hours and a maximum of 24 hours and puts gentle pressure on your cervix with an aim to softening and opening your cervix enough to stimulate labour or allow for your waters to be broken.
The balloon catheter may fall out by itself or require removal by a midwife within 24 hours.
Are there any risks of the cervical ripening balloon?
The insertion procedure can be uncomfortable but it should not be painful. The Balloon Catheter can also cause abdominal cramping which may last for a few hours. This can be managed at home with Paracetamol and/or a bath. If these methods do not help then you can contact Triage at Aberdeen Maternity Hospital on 01224 558855 for any advice and support.
Going Home after Cervical Ripening Balloon Catheter
During the time you are at home, you can do things as you would normally, for example, showering, bathing or walking. However, please avoid intercourse. After going to the toilet please wash your hands, make sure the catheter is clean and change underwear regularly.
If you have any of the following:
- Vaginal bleeding.
- Painful contractions.
- Concerns about the baby’s movements.
- Difficulty in passing urine.
- You feel unwell.
- Your waters break.
- The balloon falls out.
Please call Triage & Induction of Labour Suite on 01224 558855 where a midwife will discuss your symptoms and advise you appropriately. You will be given a time to return to Induction Suite/Labour ward for the removal of the balloon catheter no later than 24 hours following insertion.
Prostaglandin
Prostaglandin is a hormone that is naturally produced by the body. It is involved in starting labour. There are two methods used to deliver an artificial version of prostaglandin.
Firstly a pessary known as Propess® is inserted into the vagina where it releases the hormone slowly over 24 hours. It can be removed earlier if labour starts or there are concerns about you or your baby’s health. If upon removal of the Propess®, the cervix is still not favourable to break your waters or is not suitable for a cook balloon catheter then after 6 hours a tablet called Prostin® is inserted into the vagina. You will then be re-examined 6 hours after the first tablet and if the cervix is still not favourable then a second Prostin® will be inserted.
You will have to stay in hospital if these methods are used, as your baby will need to be monitored every four to six hours. Between monitoring you will be encouraged to mobilise or use the birthing balls as being active can help to encourage labour to start.

Propess®

Prostin®
Please be aware that the process of softening and opening the cervix can take up to four to five days and in some cases may not work. In this instance the team will discuss your options with you, which may be a caesarean section (Research suggests this will occur in around 6% of cases).
When the cervix is ‘favourable’ (the cervix is dilated) to have the waters around the baby broken, known as Artificial Rupture of Membranes (ARM) you will be transferred to labour ward as soon as a midwife becomes available. We aim for this to be as soon as possible however depending on clinical activity at the time. While you are waiting to be admitted to Labour ward we may offer you extra assessments and monitoring of your baby depending on your reason for induction.
Are there any risks of the Prostaglandin (Prostin®)?
Inserting the prostaglandin pessary can be uncomfortable. Prostaglandin can cause soreness in and around the vagina. It can also cause strong contractions, which can be painful; having these contractions does not always mean that you are in labour. Your midwife will discuss ways to help you manage this.
On rare occasions prostaglandins can cause the uterus to contract too frequently (around 10%) and this may affect the pattern of the baby’s heartbeat. This is usually treated by giving a drug that helps the uterus to relax. Sometimes the uterus continues to contract too frequently and there are concerns about baby’s oxygen levels (around 8%), which may mean an emergency intervention is required which may include caesarean section).
What happens when I go to Labour Ward?
Artificial Rupture of the Membranes (ARM)
When the cervix is soft, open to around two to three centimetres and the baby’s head is engaged in the pelvis, it should be possible to break the waters around the baby. This procedure is carried out by using a small plastic hook which releases the water and allows the pressure of the baby’s head to press on the cervix and stimulates contractions. It will not harm you or your baby. The procedure may be uncomfortable but it should not be painful.
You will usually be offered the artificial oxytocin hormone drip (Syntocinon®) immediately but if you have laboured in a previous pregnancy you may choose to wait some time to see if contractions start. You may also choose if this is your first baby to wait up to 4 hours to see if contractions start but this may lengthen the time you are in labour.
Hormone Drip (Syntocinon®)
Sometimes prostaglandin and/or breaking the waters is enough to start a labour, however in the instances when this doesn’t happen we offer a hormone drip. This is an artificial form of the hormone oxytocin that causes your uterus to contract. It is given through a drip into a vein in your arm called a cannula. It is usually used when your waters have broken, either naturally or artificially and your contractions have not started themselves.
The dose of the medication is adjusted according to how your labour is progressing and is increased until your uterus is contracting regularly and strongly. Women respond differently to how well the drip works on contractions and it also depends on how ready your body is for the labour process. The aim is for the uterus to contract regularly until the birth of your baby.
If you require Syntocinon® during labour, we would advise that your baby’s heart rate is monitored continuously using a CTG monitor. Your ability to walk around will be limited by the drip and monitor, however your midwife will support you to stand up, sit on a chair or birthing ball. The contractions can feel quite strong with this method of induction, but the midwife will be able to discuss with you how you are coping, and give you information about different methods of pain relief.
Are there any risks to hormone drip? (Syntocinon®)
As with prostaglandin, the main risk is that the uterus can contract too strongly/frequently and affect the baby’s heartbeat. Reducing the rate of the Syntocinon can have an immediate effect on easing the contractions, which will improve the baby’s heartbeat. If the baby’s heartbeat does not recover, the doctors may decide that your baby needs to be delivered by the quickest possible method to avoid risks of lack of oxygen, this may be by ventouse, forceps or a caesarean section.
What happens if induction of labour doesn’t work?
In a small number of cases (around 6%), induction of labour is not successful following repeated attempts. If this were to happen, your care would be discussed with a consultant obstetrician and a plan made with you as to what to do next. It may be that a caesarean section is recommended or resting for a few days and starting the process again.
Why might my induction be postponed?
Unfortunately there can be occasions where we may have to postpone your induction of labour. Sometimes when the hospital is very busy, the midwives and doctors have to prioritise the women who are booked for induction of labour. Your induction may be postponed if there is another woman that has a greater need at the time you have been given. Your induction may also be postponed if the workload on the labour ward means there is no midwife available to care for you at the time you have been given. We understand that you may be upset if your induction has been postponed and we will try and arrange for any delay to be as minimal as possible, depending on your circumstances and those of the labour ward. Our priority is to ensure that when we start your induction we can look after you and your baby safely.
If your induction has been delayed, we may ask you to attend the Aberdeen Maternity Hospital or your local community maternity unit to carry out some additional monitoring of you and your baby, such as a Cardiotocograph (CTG) which monitors your baby’s heartbeat. If there are no concerns following these checks you will be able to go back home and await induction.
